Seasonal Affective Disorder - The Basics
So, why do I say that it is not surprising the exposure to bright light alleviates both seasonal depression and other kinds of depression, and that different mechanisms may be involved?
In mammals, apart from visual photoreception (that is, image formation), there is also non-visual photoreception. The receptors of the former are the rods and cones that you all learned about in middle school. The receptors for the latter are a couple of thousand Retinal Ganglion Cells (RGCs) located in the retina in each eye. Each of these cells expresses a photopigment melanopsin (the cryptochrome challenger apparently lost the contest about a year ago after several years of frantic research by proponents of both hypotheses).
The axons – nerve processes – from these cells go to and make connections in three parts of the brain. One is the brain center that controls pupillary reflex – when the light is bright the pupils constrict, while in the dark the pupils dilate.
The second is the brain center involved in the control of mood. There is still a lot to work out about this center, but that is probably the place where exposure to light helps alleviate regular, i.e., non-seasonal depression.
The third place where these RGCs project is the suprachiasmatic nucleus (SCN) – the main circadian pacemaker in the mammalian circadian system. The first light of dawn perceived by the eyes tells the SCN that it is day. Likewise, at dusk, the gradual decrease in light intensity perceived by these RGCs signals to the SCN that night is about to start.
Much of the work on seasonal depression (SAD) suggests that it appears in response to the changes in daylength – the photoperiod. While other aspects of the weather, e.g., brightness, temperature, etc., may modulate the response, the basic mechanism appears to be the same way other mammals time their seasonal activities, including breeding, migration, molting and hibernation. Recent studies indicate that other mammals also suffer from winter depresssion, which is triggered by long night and short days (that last link is to a really cool study - perhaps I should write a separate post just on that!).
What is important to keep in mind is that total amount of received light, its intensity and quality, do not matter in photoperiodic response in mammals. What matter is the duration of the night AS PERCEIVED BY THE SCN. One can fool the SCN by, for instance mimicking a long summer day with skeleton photoperiods (a light pulse in the morning and a pulse in the afternoon) – the clock perceives only two pulses of light (a total of a couple of hours of illumination), yet interprets is as a long day.
The output of the SCN, among else, is a projection to the superior cervical ganglia (SCG) in the upper neck region, which are part of the sympathetic (autonomic or vegetative) nervous system. The SCGs, in turn, project their axons onto the pineal gland where release of nor-epinephrine controls the synthesis and secretion of the pineal hormone melatonin. So, whenever the SCN ‘thinks’ it is night, the pineal secretes melatonin into the bloodstream.
During the day, the SCN inhibits the secretion of melatonin. The duration of melatonin secretion is the signal for the duration of the night. This signals is then “read and interpreted” by other parts of the brain that trigger changes in development, morphology, physiology, reproduction and behavior in a seasonally appropriate manner. So, it is the duration of exposure to melatonin, not any direct hormonal activity of melatonin, that is the key to seasonal phenomena.
Here is a schematic of the melatonin profile in the blood of normal people in summer and winter:

 Such profiles are very important for fitness (survival and reproduction) in hamsters, sheep, deer and most other mammals. Humans are not so strikingly seasonal – we breed throughout the year – but our distant ancestors certainly were. Some traces of the seasonality of our ancestors can be seen. For instance we crave different foods in different seasons, put on or lose weight seasonally, etc. The best evidence for the human seasonality is the existence of SAD. Just like other mammals, we get slow, grouchy, and in severe cases, clinically depressed during the winter (yes, I know, there are some rare people who are opposite – depressed in summer, but they are seasonal, too, and their SAD is also due to photoperiodic time measurement).
Such profiles are very important for fitness (survival and reproduction) in hamsters, sheep, deer and most other mammals. Humans are not so strikingly seasonal – we breed throughout the year – but our distant ancestors certainly were. Some traces of the seasonality of our ancestors can be seen. For instance we crave different foods in different seasons, put on or lose weight seasonally, etc. The best evidence for the human seasonality is the existence of SAD. Just like other mammals, we get slow, grouchy, and in severe cases, clinically depressed during the winter (yes, I know, there are some rare people who are opposite – depressed in summer, but they are seasonal, too, and their SAD is also due to photoperiodic time measurement).
How does exposure to bright light alleviate SAD? Most humans have an inherent freerunning period (tau) of their circadian clock somewhat longer than 24 hours – around 25, actually. Thus, the two figures I drew above are idealized – very few people have profiles exactly like that. We tend to wake up some hours after dawn. We sleep indoors in relatively dark rooms, perhaps under covers, with our eyes closed. The RGCs do not perceive the first light of dawn at the time of dawn but some time afterwards. Thus, the SCN entrains to the environmental light-dark cycle with a slight delay. Most humans are mild “owls” in this respect. And even when we get up, we expose ourselves only to the relatively weak artificial light, or the dim light of a dark and dreary winter morning.
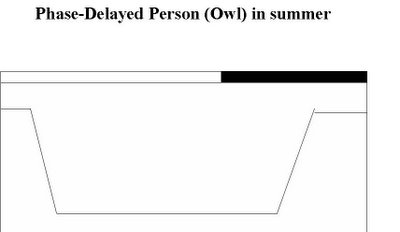
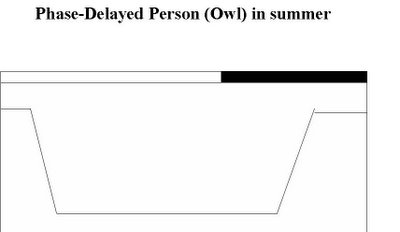
In the evening, most people do not go to bed at dusk, but switch on the lights (curse you, Edison!) and go to bed much later – often around midnight. We phase-delay our clocks with our daily behaviors. Yet, the artificial light is not sufficiently intense to shut down the secretion of melatonin. What you get is something like this – an artificially lengthened night and even longer duration of the melatonin signal than what the actual duration of night warrants:

By exposure to very bright light (a ‘light-box’ that you can buy online) in the morning, we phase-advance our clocks every morning, just enough to place ourselves into a more normal phase. High intensity is needed as the speed and size of phase resetting is dependent on light intensity. This way, we reduce the perceived duration of the night to what it really is (instead of the artificially lengthened night), thus alleviating some of the mood-related effects of short photoperiods.
 “Larks” are people whose clocks run with a period at or shorter than 24 hours and who are, thus, somewhat phase-advanced in relation to the environmetal light-dark cycles. The strategy for “larks” is to expose the RGCs to bright light in the evening, thus phase-delaying the clock and, again, reducing the perceived duration of night to the actual duration of night, hopefully eliminating mood-altering effects of long winter nights:
“Larks” are people whose clocks run with a period at or shorter than 24 hours and who are, thus, somewhat phase-advanced in relation to the environmetal light-dark cycles. The strategy for “larks” is to expose the RGCs to bright light in the evening, thus phase-delaying the clock and, again, reducing the perceived duration of night to the actual duration of night, hopefully eliminating mood-altering effects of long winter nights:
I

Melatonin supplements are often used in treatment of clock-related disorders. Melatonin has been suggested to treat jet-lag, effects of night-work and shift-work (“shift-lag”) and various clock-related insomnias. But beware – melatonin is also a signal of season.
I have not seen a study of this, but here is something that, in theory, can happen. If you are an extreme night owl, i.e., phase-delayed and try to reset your clock by taking melatonin earlier in the evening than your normal (i.e., very late) bed-time, what is going to happen?
 Even if you do this in the middle of summer, the melatonin supplement will prolong the nightly melatonin signal (exogenous melatonin in early night + endogenous melatonin during late night). Your brain will interpret this as an abrupt onset of very long winter nights. If you are susceptible to winter depression (and if I remember some studies correctly, owls are more susceptible to SAD than larks), you will artificially trigger SAD in the middle of the summer. So, beware!
Even if you do this in the middle of summer, the melatonin supplement will prolong the nightly melatonin signal (exogenous melatonin in early night + endogenous melatonin during late night). Your brain will interpret this as an abrupt onset of very long winter nights. If you are susceptible to winter depression (and if I remember some studies correctly, owls are more susceptible to SAD than larks), you will artificially trigger SAD in the middle of the summer. So, beware!
Now, you may understand why are people who live in very high latitudes chronically depressed. After all, they are exposed to a continuous night that lasts for several months! One wonders if the reindeer are depressed, too.
What I outlined here is just the very basic mechanism of SAD - the textbook version. There are, as one should expect, many more details, complications and strange data out there. Those are, frankly, outside my domain of expertise. I am a bird kind of guy, after all. So, if you want more details, or medical advice, you will be better off to ask somebody who does research on (and clinical work with) human subjects, or at least on mammals.
In mammals, apart from visual photoreception (that is, image formation), there is also non-visual photoreception. The receptors of the former are the rods and cones that you all learned about in middle school. The receptors for the latter are a couple of thousand Retinal Ganglion Cells (RGCs) located in the retina in each eye. Each of these cells expresses a photopigment melanopsin (the cryptochrome challenger apparently lost the contest about a year ago after several years of frantic research by proponents of both hypotheses).
The axons – nerve processes – from these cells go to and make connections in three parts of the brain. One is the brain center that controls pupillary reflex – when the light is bright the pupils constrict, while in the dark the pupils dilate.
The second is the brain center involved in the control of mood. There is still a lot to work out about this center, but that is probably the place where exposure to light helps alleviate regular, i.e., non-seasonal depression.
The third place where these RGCs project is the suprachiasmatic nucleus (SCN) – the main circadian pacemaker in the mammalian circadian system. The first light of dawn perceived by the eyes tells the SCN that it is day. Likewise, at dusk, the gradual decrease in light intensity perceived by these RGCs signals to the SCN that night is about to start.
Much of the work on seasonal depression (SAD) suggests that it appears in response to the changes in daylength – the photoperiod. While other aspects of the weather, e.g., brightness, temperature, etc., may modulate the response, the basic mechanism appears to be the same way other mammals time their seasonal activities, including breeding, migration, molting and hibernation. Recent studies indicate that other mammals also suffer from winter depresssion, which is triggered by long night and short days (that last link is to a really cool study - perhaps I should write a separate post just on that!).
What is important to keep in mind is that total amount of received light, its intensity and quality, do not matter in photoperiodic response in mammals. What matter is the duration of the night AS PERCEIVED BY THE SCN. One can fool the SCN by, for instance mimicking a long summer day with skeleton photoperiods (a light pulse in the morning and a pulse in the afternoon) – the clock perceives only two pulses of light (a total of a couple of hours of illumination), yet interprets is as a long day.
The output of the SCN, among else, is a projection to the superior cervical ganglia (SCG) in the upper neck region, which are part of the sympathetic (autonomic or vegetative) nervous system. The SCGs, in turn, project their axons onto the pineal gland where release of nor-epinephrine controls the synthesis and secretion of the pineal hormone melatonin. So, whenever the SCN ‘thinks’ it is night, the pineal secretes melatonin into the bloodstream.
During the day, the SCN inhibits the secretion of melatonin. The duration of melatonin secretion is the signal for the duration of the night. This signals is then “read and interpreted” by other parts of the brain that trigger changes in development, morphology, physiology, reproduction and behavior in a seasonally appropriate manner. So, it is the duration of exposure to melatonin, not any direct hormonal activity of melatonin, that is the key to seasonal phenomena.
Here is a schematic of the melatonin profile in the blood of normal people in summer and winter:

 Such profiles are very important for fitness (survival and reproduction) in hamsters, sheep, deer and most other mammals. Humans are not so strikingly seasonal – we breed throughout the year – but our distant ancestors certainly were. Some traces of the seasonality of our ancestors can be seen. For instance we crave different foods in different seasons, put on or lose weight seasonally, etc. The best evidence for the human seasonality is the existence of SAD. Just like other mammals, we get slow, grouchy, and in severe cases, clinically depressed during the winter (yes, I know, there are some rare people who are opposite – depressed in summer, but they are seasonal, too, and their SAD is also due to photoperiodic time measurement).
Such profiles are very important for fitness (survival and reproduction) in hamsters, sheep, deer and most other mammals. Humans are not so strikingly seasonal – we breed throughout the year – but our distant ancestors certainly were. Some traces of the seasonality of our ancestors can be seen. For instance we crave different foods in different seasons, put on or lose weight seasonally, etc. The best evidence for the human seasonality is the existence of SAD. Just like other mammals, we get slow, grouchy, and in severe cases, clinically depressed during the winter (yes, I know, there are some rare people who are opposite – depressed in summer, but they are seasonal, too, and their SAD is also due to photoperiodic time measurement).How does exposure to bright light alleviate SAD? Most humans have an inherent freerunning period (tau) of their circadian clock somewhat longer than 24 hours – around 25, actually. Thus, the two figures I drew above are idealized – very few people have profiles exactly like that. We tend to wake up some hours after dawn. We sleep indoors in relatively dark rooms, perhaps under covers, with our eyes closed. The RGCs do not perceive the first light of dawn at the time of dawn but some time afterwards. Thus, the SCN entrains to the environmental light-dark cycle with a slight delay. Most humans are mild “owls” in this respect. And even when we get up, we expose ourselves only to the relatively weak artificial light, or the dim light of a dark and dreary winter morning.
In the evening, most people do not go to bed at dusk, but switch on the lights (curse you, Edison!) and go to bed much later – often around midnight. We phase-delay our clocks with our daily behaviors. Yet, the artificial light is not sufficiently intense to shut down the secretion of melatonin. What you get is something like this – an artificially lengthened night and even longer duration of the melatonin signal than what the actual duration of night warrants:

By exposure to very bright light (a ‘light-box’ that you can buy online) in the morning, we phase-advance our clocks every morning, just enough to place ourselves into a more normal phase. High intensity is needed as the speed and size of phase resetting is dependent on light intensity. This way, we reduce the perceived duration of the night to what it really is (instead of the artificially lengthened night), thus alleviating some of the mood-related effects of short photoperiods.
 “Larks” are people whose clocks run with a period at or shorter than 24 hours and who are, thus, somewhat phase-advanced in relation to the environmetal light-dark cycles. The strategy for “larks” is to expose the RGCs to bright light in the evening, thus phase-delaying the clock and, again, reducing the perceived duration of night to the actual duration of night, hopefully eliminating mood-altering effects of long winter nights:
“Larks” are people whose clocks run with a period at or shorter than 24 hours and who are, thus, somewhat phase-advanced in relation to the environmetal light-dark cycles. The strategy for “larks” is to expose the RGCs to bright light in the evening, thus phase-delaying the clock and, again, reducing the perceived duration of night to the actual duration of night, hopefully eliminating mood-altering effects of long winter nights:I


Melatonin supplements are often used in treatment of clock-related disorders. Melatonin has been suggested to treat jet-lag, effects of night-work and shift-work (“shift-lag”) and various clock-related insomnias. But beware – melatonin is also a signal of season.
I have not seen a study of this, but here is something that, in theory, can happen. If you are an extreme night owl, i.e., phase-delayed and try to reset your clock by taking melatonin earlier in the evening than your normal (i.e., very late) bed-time, what is going to happen?
 Even if you do this in the middle of summer, the melatonin supplement will prolong the nightly melatonin signal (exogenous melatonin in early night + endogenous melatonin during late night). Your brain will interpret this as an abrupt onset of very long winter nights. If you are susceptible to winter depression (and if I remember some studies correctly, owls are more susceptible to SAD than larks), you will artificially trigger SAD in the middle of the summer. So, beware!
Even if you do this in the middle of summer, the melatonin supplement will prolong the nightly melatonin signal (exogenous melatonin in early night + endogenous melatonin during late night). Your brain will interpret this as an abrupt onset of very long winter nights. If you are susceptible to winter depression (and if I remember some studies correctly, owls are more susceptible to SAD than larks), you will artificially trigger SAD in the middle of the summer. So, beware!Now, you may understand why are people who live in very high latitudes chronically depressed. After all, they are exposed to a continuous night that lasts for several months! One wonders if the reindeer are depressed, too.
What I outlined here is just the very basic mechanism of SAD - the textbook version. There are, as one should expect, many more details, complications and strange data out there. Those are, frankly, outside my domain of expertise. I am a bird kind of guy, after all. So, if you want more details, or medical advice, you will be better off to ask somebody who does research on (and clinical work with) human subjects, or at least on mammals.





1 Comments:
And that is, no doubt, why my sleep specialist (DSPS) wouldn't start me on melatonin before I'd got hold of a light box. You don't want melatonin for all those extra hours. The light chases the melatonin away.
BTW, where I live, melatonin is by extra-strict prescription only. "My" light box was free, on permanent loan as a medical necessity.
Post a Comment
<< Home